TIM-3 therapy for Alzheimer’s is emerging as a pioneering advance in Alzheimer’s disease research, aiming to leverage the immune system for enhanced cognitive improvement. Recent studies have shown that targeting the TIM-3 molecule, known for its role in inhibiting microglia function, could unlock new pathways for the clearance of amyloid plaques in the brain. By disrupting the inhibitory mechanisms of TIM-3, researchers believe that these immune cells may be stimulated to reclaim lost functionality, potentially reversing memory loss in affected individuals. This innovative approach has continued dialogues about immune checkpoint inhibitors, which have traditionally been aligned with cancer treatment strategies, and their role in neurodegenerative conditions. As we delve deeper into the intricacies of TIM-3 therapy, the promise it holds in altering the landscape of Alzheimer’s has never been more significant.
Exploring innovative methods to combat Alzheimer’s disease, TIM-3 inhibition represents a novel frontier in neuroimmunology. This groundbreaking approach takes advantage of the body’s own immune response, aiming to reactivate the functions of microglia, the brain’s resident immune cells, which are pivotal in maintaining cognitive health. By blocking the TIM-3 pathway, researchers are investigating how to harness these cells to efficiently target and dismantle amyloid-beta plaques, thus promoting synaptic health. As this research evolves, it not only redefines our understanding of Alzheimer’s pathology but also bridges concepts from cancer immunotherapy to neurodegenerative disease management. The potential for significant cognitive recovery through this method highlights a transformative shift in therapeutic strategies that could change the future for millions facing Alzheimer’s.
Understanding TIM-3 and Its Role in Alzheimer’s Disease
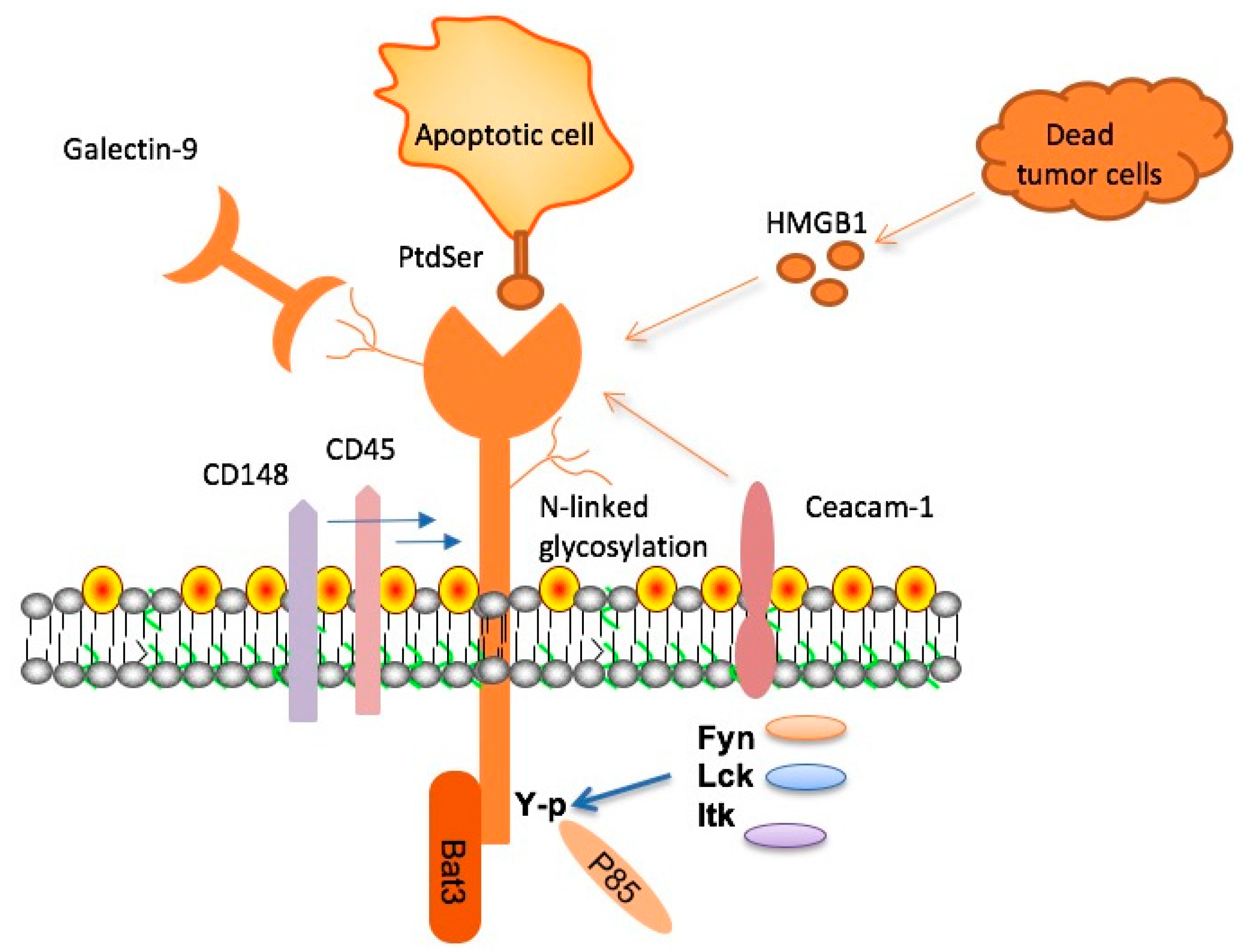
TIM-3, or T cell immunoglobulin and mucin-domain containing-3, is a crucial checkpoint molecule that plays a significant role in regulating immune responses. In the context of Alzheimer’s disease, TIM-3 is expressed on microglia, the brain’s immune cells, and is known to inhibit their ability to clear amyloid-beta plaques. This accumulation of plaques is a hallmark of Alzheimer’s disease, leading to neurodegeneration and cognitive decline. Research indicates that TIM-3 expression is significantly higher in microglia of Alzheimer’s patients, making it a key focus for therapeutic strategies aimed at restoring cognitive function.
Research led by a team at Harvard has demonstrated that deleting TIM-3 from microglia can effectively enhance plaque clearance and improve cognitive performance in mice models of Alzheimer’s disease. This process underscores the importance of the immune system in maintaining brain health, and highlights how unraveling the complexities of microglia function is essential in developing effective Alzheimer’s treatments. By targeting TIM-3, we may unlock new pathways for cognitive improvement in Alzheimer’s patients, potentially transforming future treatment protocols.
Potential of TIM-3 Therapy in Treating Alzheimer’s
The prospect of using TIM-3 therapy for Alzheimer’s disease represents a novel approach in treating this complex condition. TIM-3 therapy could involve the use of anti-TIM-3 antibodies or small molecules that block the inhibitory effects of TIM-3, effectively unleashing the potential of microglia to clear amyloid plaques. This targeted therapy aims not only to reduce plaque accumulation but also to mitigate the associated cognitive impairments. Given that current Alzheimer’s treatments have shown only minimal effectiveness, TIM-3 therapy offers hope for a more robust solution.
By repurposing existing immunotherapy strategies, traditionally used for cancer treatment, researchers are seeking new ways to leverage the immensity of immune checkpoint inhibitors against Alzheimer’s. The transition of these cancer-fighting strategies to brain health exemplifies the innovative thinking necessary to tackle Alzheimer’s disease. In essence, TIM-3 therapy could herald a new era in achieving cognitive improvement and slowing the progression of Alzheimer’s, ultimately benefiting millions who face this debilitating disease.
Microglia’s Function and Alzheimer’s Disease
Microglia serve as the brain’s intrinsic immune responders, playing vital roles not just in immune defense but also in synaptic pruning and overall CNS homeostasis. In the event of disease, such as Alzheimer’s, the dysregulation of this neuroimmune response becomes evident, with microglia failing to perform their function of clearing amyloid plaques. This impairment is exacerbated by the upregulation of checkpoint molecules like TIM-3, which alters their state from responding to threats to a more homeostatic, inactive form. Understanding microglial function is crucial for researchers delving into Alzheimer’s pathology.
In Alzheimer’s, the improper activation and function of microglia contribute heavily to disease progression. The challenge lies in re-establishing the balance in microglial activity, enabling these cells to effectively eliminate harmful plaques without triggering further neuroinflammation. This delicate balance is pivotal; ensuring microglia can engage properly is essential for reversing or mitigating cognitive decline. Through ongoing research, strategies targeting microglial function are being explored to potentially rejuvenate the brain’s defenses against Alzheimer’s.
Linking TIM-3 and Alzheimer’s Cognitive Function
Recent studies have uncovered a compelling link between TIM-3 expression in microglia and cognitive function in Alzheimer’s disease models. The overexpression of TIM-3 not only inhibits plaque clearance but also correlates with worsened cognitive outcomes, highlighting its role as a biomarker for Alzheimer’s progression. By targeting TIM-3, researchers are proposing a dual approach to therapy: reducing amyloid burden and enhancing memory function simultaneously. This integrative strategy could redefine treatment methods, shifting from mere plaque reduction to holistic cognitive health improvement.
Moreover, addressing TIM-3 levels in Alzheimer’s pathology may facilitate significant strides in understanding not only the mechanisms of cognitive decline but also potential reparative strategies. As the research evolves, comprehensive trials could potentially reveal the intricate relationship between TIM-3 modulation and cognitive restoration. By employing robust methodologies, the aim is to translate promising findings from mouse models into viable therapeutic options for patients afflicted by Alzheimer’s.
The Role of Checkpoint Inhibitors in Alzheimer’s Therapy
Checkpoint inhibitors, widely recognized in the realm of cancer immunotherapy, have emerged as potential allies in the battle against Alzheimer’s disease. The therapeutic application of these agents can modulate the hyperactive signaling that inhibits vital immune responses, such as the action of microglia against neurotoxic plaque buildup. This innovative strategy not only applies existing knowledge from oncology but also tailors it to target the unique pathophysiological features of neurodegenerative diseases, thus expanding the frontier of therapeutic options.
Through the careful adaptation of immune checkpoint strategies, researchers are beginning to understand how to safely and effectively harness the brain’s immune response. The potential of using checkpoint inhibitors, like anti-TIM-3 antibodies, presents a transformative opportunity to enhance brain health outcomes by mitigating Alzheimer’s disease’s cognitive repercussions. The intersection of cancer treatment strategies and neurodegenerative research underscores the importance of interdisciplinary approaches in medicine, with the goal of reversing the tide against Alzheimer’s.
Clinical Implications of TIM-3 Modulation
The clinical implications of modulating TIM-3 expression in Alzheimer’s patients are profound. Recent findings suggest that inhibiting TIM-3 may enhance microglial function, potentially leading to improved cognitive outcomes in patients suffering from Alzheimer’s. As therapeutic trials begin to investigate the feasibility of TIM-3-targeted therapies, the hope is high that these adaptations will result in effective intervention strategies, enabling clinicians to provide better support and treatment for their patients.
Importantly, this modulation of TIM-3 could lead to advancements not only in understanding patient-specific variations in Alzheimer’s pathology but also in creating personalized medicine approaches. With the integration of genetic profiling and biomarker analysis, therapies could be customized to maximize efficacy while minimizing side effects. As the scientific community gathers more evidence, the aim is to bridge the gap between innovative research and tangible clinical applications for vulnerable populations suffering from Alzheimer’s.
Future Directions in Alzheimer’s Disease Research
The future directions in Alzheimer’s disease research point towards a multifaceted approche that includes innovative mechanisms such as TIM-3 therapy. As researchers delve deeper into the complexities of immune responses in the brain, strategies targeting microglial function stand to revolutionize how Alzheimer’s disease is treated. By reshaping our understanding of immune system involvement in neurodegeneration, future studies are poised to develop therapies that could significantly alter disease trajectories.
Collaboration across disciplines will be essential in propelling Alzheimer’s research forward. Building on insights gained from cancer immunotherapy, novel strategies that adapt these principles for neurodegenerative contexts will likely emerge. As the scientific community works towards a unified understanding of Alzheimer’s mechanisms, the focus on TIM-3 and similar checkpoint targets could provide leads for groundbreaking interventions, fostering hope for those affected by this impactful disease.
Cognitive Improvement Through Targeted Therapies
The drive for cognitive improvement in Alzheimer’s patients hinges on targeted therapies that address the root causes of neurodegeneration. As research into TIM-3 therapy unfolds, the approach aims not only to clear amyloid plaques but also to restore cognitive functions that are increasingly impaired over time. This dual focus allows for a robust framework in which symptomatic relief can be achieved while also addressing the underlying pathophysiology of the disease.
In future therapeutic settings, leveraging agents that can effectively modulate microglial activity and enhance their plaque-clearing abilities will be paramount. Successful cognitive improvement hinges on understanding these interactions and developing drugs that reflect these complex interplay dynamics. With time, care, and continued research, the hope is to translate these scientific breakthroughs into tangible benefits for Alzheimer’s patients, making substantial strides towards improved cognitive outcomes.
Progress in Alzheimer’s Research and Clinical Trials
Ongoing progress in Alzheimer’s research continues to illuminate pathway connections that may lead to successful therapeutic interventions. The clinical trial landscape is actively evaluating various approaches to targeting TIM-3, as well as other molecular pathways implicated in Alzheimer’s pathology. Each trial contributes valuable insights, moving the field towards not only finding potential solutions but also refining our understanding of the biological underpinnings of the disease.
As new evidence emerges from animal studies and human clinical trials, it will be crucial to remain adaptable. Learning from the outcomes of these investigations will guide future research directions, driving innovation within therapies. With the potential of TIM-3 therapy on the horizon, the Alzheimer’s research community is optimistic about potential breakthroughs that could redefine patient care and support, enhancing the quality of life for individuals affected by this disease.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 checkpoint molecule to enhance the function of microglia, the brain’s immune cells. By inhibiting TIM-3, this therapy aims to restore the ability of microglia to clear amyloid plaques associated with Alzheimer’s, potentially improving cognitive function.
How does TIM-3 impact microglia function in Alzheimer’s?
In Alzheimer’s disease, TIM-3 inhibits microglia from attacking amyloid plaques. This inhibition leads to the accumulation of plaques, which are harmful to cognitive function. By blocking TIM-3, researchers hope to reactivate microglia’s ability to phagocytose these plaques, thereby promoting cognitive improvement.
What role does TIM-3 play in Alzheimer’s disease research?
TIM-3 is a significant focus in Alzheimer’s disease research as it has been identified as a genetic risk factor for late-onset Alzheimer’s. Studies show that higher levels of TIM-3 on microglia correlate with reduced plaque clearance, highlighting its potential as a therapeutic target for enhancing cognitive abilities.
Can TIM-3 therapy improve cognitive function in Alzheimer’s patients?
Preclinical studies on mice suggest that TIM-3 therapy can lead to cognitive improvements by enabling microglia to effectively clear amyloid plaques from the brain. While human studies are needed, these findings raise optimism for potential cognitive benefits in Alzheimer’s patients.
How does the removal of TIM-3 affect Alzheimer’s treatment strategies?
Removing TIM-3 enhances microglial activity and plaque clearance, providing a novel strategy for treating Alzheimer’s. This approach can differentiate from traditional anti-amyloid therapies that have shown limited efficacy and may lead to better outcomes for cognitive function.
What is the mechanism of action for TIM-3 therapy in Alzheimer’s disease?
TIM-3 therapy works by blocking the inhibitory signals of TIM-3 on microglia, allowing these immune cells to engage and eliminate harmful amyloid beta plaques. This mechanism aims to reverse some cognitive deficits associated with Alzheimer’s disease.
What potential does TIM-3 therapy have compared to existing Alzheimer’s treatments?
TIM-3 therapy holds significant potential as it may directly enhance the brain’s immune response to plaques, contrasting with therapies that primarily address amyloid levels without improving microglial function. This could lead to more effective treatment strategies and improved Alzheimer’s outcomes.
Are there any clinical trials for TIM-3 therapy in Alzheimer’s disease?
While preclinical studies have shown promising results in mice, clinical trials for TIM-3 therapy in humans are still in the early stages. Research teams are currently testing anti-TIM-3 antibodies in mouse models with the goal of moving towards clinical applications.
What are the challenges of implementing TIM-3 therapy for Alzheimer’s disease?
Challenges include ensuring that TIM-3 inhibitors can safely penetrate the blood-brain barrier and effectively target microglia without causing adverse effects. Additionally, understanding the long-term impacts on cognitive improvement is crucial for successful therapy.
How long has TIM-3 therapy research been underway for Alzheimer’s?
Research on TIM-3 therapy for Alzheimer’s disease has been ongoing for about five years. This entails extensive studies to assess its effects on microglia function and plaque clearance in disease models.
| Key Point | Details |
|---|---|
| TIM-3 therapy for Alzheimer’s | Potential treatment using an immune checkpoint molecule that has shown promise in cancer therapy. |
| Role of TIM-3 | TIM-3 inhibits microglia from attacking amyloid plaques in the brain, contributing to Alzheimer’s progression. |
| Mouse Model Research | Studies involved mice genetically modified to delete the TIM-3 gene, leading to improved memory and plaque clearance. |
| Potential Benefits | Reducing plaque accumulation and restoring cognitive function in models of late-onset Alzheimer’s disease. |
| Future Directions | Next steps include testing human anti-TIM-3 in mouse models to evaluate its effectiveness in halting plaque development. |
Summary
TIM-3 therapy for Alzheimer’s is emerging as a promising avenue for treatment, leveraging the insights gained from cancer therapies. This innovative approach focuses on the TIM-3 molecule’s role in regulating the brain’s immune response, which may allow for the effective clearance of amyloid plaques implicated in Alzheimer’s disease. Ongoing research aims to establish the efficacy of TIM-3 blockade in human models, potentially revolutionizing how we address this debilitating condition.