AI predicting brain cancer recurrence represents a groundbreaking advancement in the realm of pediatric oncology. A recent study conducted by Harvard researchers reveals that artificial intelligence outperforms traditional methods in anticipating relapse risk for children suffering from brain tumors, specifically pediatric gliomas. By employing an innovative temporal learning approach, this AI tool analyzes a sequence of brain scans, enhancing its accuracy in detecting the subtle changes that indicate potential recurrence. The implications for childhood cancer prognosis are significant, as improved predictive capabilities could lead to individualized treatment plans and less intrusive follow-up procedures. As this research progresses, the integration of AI in medicine could revolutionize brain cancer imaging and management for young patients.
Artificial intelligence is rapidly transforming medical practices, particularly in predicting the recurrence of brain tumors in pediatric patients. This innovative technology, particularly using techniques like temporal learning, allows for a comprehensive analysis of multiple imaging studies over time. Researchers are now able to closely monitor childhood cancer prognosis by identifying at-risk individuals more accurately than ever before. The potential for early detection of relapse in conditions like pediatric gliomas may pave the way for tailored treatment approaches, significantly improving patient outcomes. Such advancements in brain cancer detection methodologies promise to elevate standards of care and ease the burden on families navigating the complexities of childhood cancer.
The Role of AI in Predicting Brain Cancer Recurrence
In recent developments, AI technology has emerged as a formidable tool in predicting the recurrence of brain tumors, particularly in pediatric gliomas. Traditional methods often fall short in their accuracy, leaving families and healthcare providers in uncertainty regarding the optimal follow-up care for young patients. An AI model, trained on longitudinal brain scans, has demonstrated the ability to forecast relapse risks more effectively, providing a glimpse of hope in the challenging landscape of childhood cancer prognosis.
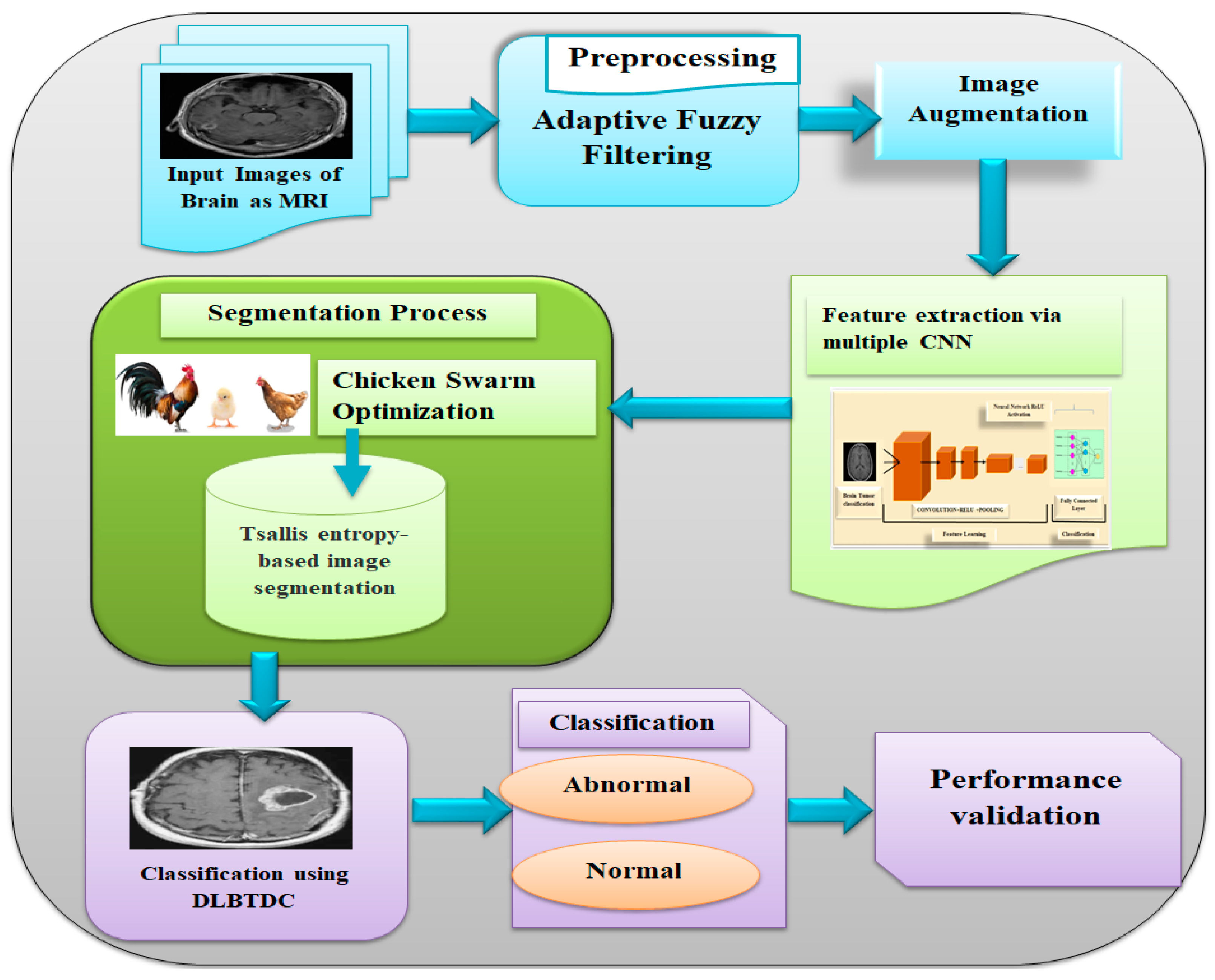
Researchers have highlighted how incorporating AI into medical imaging can transform the management of pediatric brain cancers. By utilizing temporal learning techniques, the AI can analyze sequences of MR scans over time, identifying subtle changes that may indicate a shift towards relapse. This sophisticated approach allows for a more personalized treatment plan, tailored to the individual patient’s risk profile, significantly enhancing the clinical decision-making process.
Understanding Pediatric Gliomas: A Brief Overview
Pediatric gliomas are brain tumors that can be quite variable in their behavior and response to treatment. Generally considered treatable, these tumors still pose significant risks, particularly regarding recurrence. Surgery often serves as the primary treatment; however, the challenge lies in monitoring and predicting potential relapses. Conventional imaging methods may not provide the necessary insights, resulting in uncertainty for families navigating the complexities of childhood cancer treatment.
The classification of pediatric gliomas includes various types, each associated with differing prognoses and treatment approaches. From low-grade tumors, which may have a better long-term outlook, to high-grade variants that require aggressive management, understanding these distinctions is critical for the effective application of targeted therapies. AI’s potential in enhancing imaging accuracy can lead to markedly improved outcomes for children facing these daunting conditions.
Temporal Learning: A Game-Changer in Cancer Imaging
Temporal learning represents a significant advancement in the field of cancer imaging, particularly for patients undergoing treatment for pediatric gliomas. By analyzing a series of MR scans taken over time rather than focusing on single images, AI models can detect patterns and changes that may go unnoticed. This advancement is essential in providing a comprehensive view of how a tumor evolves post-surgery, ensuring that clinicians can make informed decisions regarding follow-up care.
The effectiveness of temporal learning lies in its ability to predict cancer recurrence with impressive accuracy. In the study conducted by researchers at Mass General Brigham, the AI’s ability to forecast relapses reached levels of up to 89 percent accuracy—significantly higher than traditional methods. This not only aids in identifying at-risk patients earlier but also paves the way for innovative treatment protocols that could improve overall survival rates for pediatric patients.
Implications for Childhood Cancer Prognosis and Treatment
The implications of improved prediction models using AI extend far beyond just understanding relapse risks; they carry profound effects on the prognosis and treatment strategies for childhood cancers. Enhanced imaging capabilities can lead to better stratification of patients, identifying those who may benefit from more intensive treatment versus those who could safely reduce their imaging burden. This approach not only alleviates the psychological strain on patients and families but also optimizes resource allocation in healthcare.
As the research progresses, integrating AI tools into clinical practice can also facilitate earlier interventions for high-risk patients, allowing for timely implementation of targeted therapies that could prevent the progression of the disease. Ultimately, advancing our understanding of pediatric gliomas through these data-driven techniques aligns with the overarching goal of improving survival rates and quality of life for children battling brain cancer.
Future Directions in AI and Pediatric Neuroscience
Looking ahead, the integration of AI into pediatric neuroscience holds the promise of revolutionizing how we approach brain tumor treatment and management. As research continues to validate techniques like temporal learning, there is potential for AI applications to expand beyond gliomas to other types of childhood cancers. This broader application could drive the development of standardized protocols and pave the way for personalized medicine in oncology.
Moreover, as healthcare systems continue to embrace technological advancements, it is crucial to ensure that infrastructure is in place to support the clinical implementation of these predictive models. Future clinical trials will be instrumental in assessing the practical applications of AI-driven predictions and their potential to enhance patient care in real-world settings. The journey toward integrating AI in medicine is just beginning, and its impact on pediatric neuroscience is poised to be profound.
The Importance of Multidisciplinary Collaboration in AI Research
The success of AI in predicting brain cancer recurrence hinges on robust multidisciplinary collaboration among researchers, clinicians, and data scientists. Involving diverse expertise ensures that AI models are developed with comprehensive understanding of both the technical and clinical nuances of cancer treatment. The collaborations showcased in the research conducted by Mass General Brigham exemplify how pooling knowledge from various institutions leads to breakthroughs that can directly benefit patient outcomes.
As AI technology continually evolves, sustained partnerships between academic institutions, healthcare providers, and tech innovators will be necessary. These collaborations can drive the collection of larger and more diverse datasets, fostering advancements in machine learning and ensuring the tools developed are applicable in varied clinical contexts. Ultimately, collective efforts will be key to unlocking the full potential of AI in transforming cancer care for children.
Challenges and Considerations in AI Implementation
Despite the promising outcomes of AI applications in predicting brain cancer recurrence, several challenges must be addressed before widespread clinical implementation. One of the main concerns includes the need for validation across different healthcare settings to ensure the efficacy and reliability of AI models. Furthermore, ethical considerations regarding patient data privacy and the necessity of transparency within AI algorithm decision-making processes are crucial for fostering trust among patients and clinicians.
Integrating new technology into existing healthcare frameworks can also pose logistical challenges. Healthcare providers need appropriate training to interpret AI-generated predictions effectively, and systems must accommodate the additional analysis these tools require. Addressing these hurdles is essential to ensure that the anticipated benefits of AI in pediatric cancer care are fully realized without compromising patient safety or care standards.
Long-term Monitoring and Follow-Up for Pediatric Patients
Long-term monitoring remains a cornerstone of post-treatment care in pediatric oncology, particularly for patients treated for gliomas. The enhanced prediction capabilities of AI can significantly influence how follow-up protocols are established, potentially reducing the frequency of invasive imaging for low-risk patients. By identifying those who are less likely to experience recurrence, healthcare providers can alleviate the burden on both the patients and the healthcare system.
Conversely, for those identified as high-risk through AI predictions, more aggressive follow-up and treatment strategies can be implemented, leading to timely interventions that could have life-saving implications. This strategic alignment of care based on AI-informed risk profiles allows for a more efficient healthcare model focused on patient well-being, ultimately enhancing the prognosis for children facing brain cancer.
The Future Outlook: AI’s Impact on Pediatric Oncology
As we look towards the future, the role of AI in pediatric oncology is expected to expand rapidly, shaped by ongoing research and advancements in machine learning technologies. The potential applications of AI in predicting relapse in pediatric gliomas could extend to real-time monitoring during treatment and beyond, giving clinicians powerful tools to adapt interventions based on live feedback from imaging data. This shift toward proactive care can fundamentally change the landscape of childhood cancer management.
Moreover, the integration of AI into pediatric oncology may also drive an increased interest in collaborative research efforts, leading to accelerated discoveries in treatment modalities, early detection strategies, and survivorship care. By embracing this technology and fostering a culture of innovation, healthcare providers can enhance the survival rates and quality of life for children battling childhood cancers, ultimately shaping a brighter future for pediatric patients.
Frequently Asked Questions
How does AI predict brain cancer recurrence in pediatric gliomas?
AI predicts brain cancer recurrence in pediatric gliomas by analyzing multiple brain scans over time. Using a technique called temporal learning, the AI model synthesizes findings from various scans to identify subtle changes that indicate a higher risk of relapse, achieving accuracy rates between 75-89%.
What advantages does AI have over traditional methods in predicting brain cancer relapse?
AI has significant advantages over traditional methods in predicting brain cancer relapse, particularly in pediatric gliomas. An AI tool can leverage temporal data from multiple MRI scans, leading to more accurate predictions of recurrence than single-scan assessments, which generally hover around 50% accuracy.
What role does temporal learning play in AI predictions for brain cancer imaging?
Temporal learning plays a critical role in AI predictions for brain cancer imaging by allowing the AI to analyze a sequence of images taken over time. This method enables the model to recognize patterns and changes in the brain scans that may correlate with the risk of recurrence, enhancing predictive accuracy.
Can AI in medicine improve childhood cancer prognosis?
Yes, AI in medicine has the potential to significantly improve childhood cancer prognosis by offering better predictive analytics for brain cancer recurrence in pediatric gliomas. By accurately forecasting relapse risks, AI can inform treatment plans and follow-up strategies, optimizing care and reducing undue burden on patients and families.
What future applications might arise from using AI to predict brain cancer recurrence?
Future applications of AI in predicting brain cancer recurrence include personalized treatment plans based on individual risk assessments, improved follow-up imaging protocols tailored to patient needs, and potentially the development of targeted therapies for high-risk patients, ultimately enhancing outcomes for pediatric glioma survivors.
How effective was the study on AI predicting brain cancer recurrence in pediatric patients?
The study found that the AI tool effectively predicted brain cancer recurrence in pediatric patients with up to 89% accuracy, significantly outperforming traditional methods. The combination of multiple imaging scans through temporal learning allowed for a more nuanced understanding of changes in brain tumors over time.
What is the significance of accurately predicting relapse in pediatric gliomas?
Accurately predicting relapse in pediatric gliomas is vital as it facilitates timely interventions and personalized care. Early identification of high-risk patients can lead to more effective treatment strategies and reduced stress from frequent imaging and follow-ups, ultimately improving the quality of life for affected children and their families.
| Key Point | Details |
|---|---|
| AI Prediction | An AI tool outperforms traditional methods in predicting brain cancer relapse. |
| Study Background | Conducted by researchers from Mass General Brigham and Boston Children’s Hospital, leveraging 4,000 MR scans from 715 pediatric patients. |
| Temporal Learning | A new technique that trains AI on multiple MR scans over time to identify patterns and predict recurrence. |
| Accuracy | The AI model achieved 75-89% accuracy in predicting glioma recurrence, compared to about 50% for traditional methods. |
| Future Applications | Aims to refine care through reduced imaging for low-risk patients or preemptive therapies for high-risk patients. |
| Validation Needs | Further research is needed before clinical application to confirm its effectiveness in various settings. |
Summary
AI predicting brain cancer recurrence is revolutionizing how we approach pediatric gliomas. By utilizing advanced algorithms trained on multiple brain scans, researchers are significantly enhancing the accuracy of recurrence predictions compared to traditional methods. This innovative approach holds the potential to alleviate the emotional and logistical burdens of frequent imaging for families, while also enabling tailored treatment plans that could lead to better outcomes for young patients. With ongoing validation and future clinical trials, the promising results from this study pave the way for improved management of brain cancer in children.