Maternal mortality rates in the U.S. have reached alarming levels, highlighting the urgent need for action to address this critical public health issue. Despite advancements in medical care, over 80 percent of pregnancy-related deaths are preventable, yet the United States leads high-income countries in maternal mortality. Between 2018 and 2022, these rates not only increased, but stark disparities emerged across state lines and racial demographics, raising questions about maternal health disparities. Cardiovascular disease during pregnancy has shifted to become the leading cause of these deaths, further complicating the urgent need for improved postpartum care. Understanding the systemic failures within the U.S. healthcare system is essential to combat these rising mortality rates and to ensure all mothers receive equitable care during and after pregnancy.
The rising incidence of maternal deaths during childbirth, often referred to as pregnancy-related fatalities, has become a pressing concern within the realm of public health. This increase underscores significant maternal health inequities, particularly across different racial and socio-economic groups. As cardiovascular complications take center stage as leading causes of these fatalities, the importance of comprehensive postpartum support is more critical than ever. Addressing the roots of these issues requires a reassessment of the U.S. healthcare framework, which must evolve to provide continuous care throughout pregnancy and the postpartum period. A collective effort is needed to bridge the gaps in care, ensuring that every mother has access to the resources necessary for a safe pregnancy and recovery.
Understanding Maternal Mortality Rates in the U.S.
Maternal mortality rates in the U.S. have been a troubling topic, especially as they continue to rise compared to other high-income countries. This increase can be attributed to a combination of factors including inadequate prenatal care, disparities in healthcare access, and the complexities of the U.S. healthcare system. For many women, the journey through pregnancy is marred by systemic failures that result in preventable deaths. According to recent research, over 80% of pregnancy-related deaths are avoidable, yet the statistics still paint a grim picture for maternal health across the nation.
Racial and ethnic disparities further complicate the maternal mortality landscape. African American and American Indian women face significantly higher risks compared to their white counterparts. Efforts to bridge these gaps have seen some success, yet overall improvements remain elusive. Addressing these disparities is critical not only for reducing maternal mortality rates but also for fostering a more equitable healthcare environment.
Frequently Asked Questions
What are the primary factors contributing to high maternal mortality rates in the U.S.?
High maternal mortality rates in the U.S. can be attributed to several factors, including a fragmented healthcare system, inequitable policies, and significant maternal health disparities based on race and ethnicity. Additionally, the increasing prevalence of chronic conditions like cardiovascular disease among pregnant individuals exacerbates these rates.
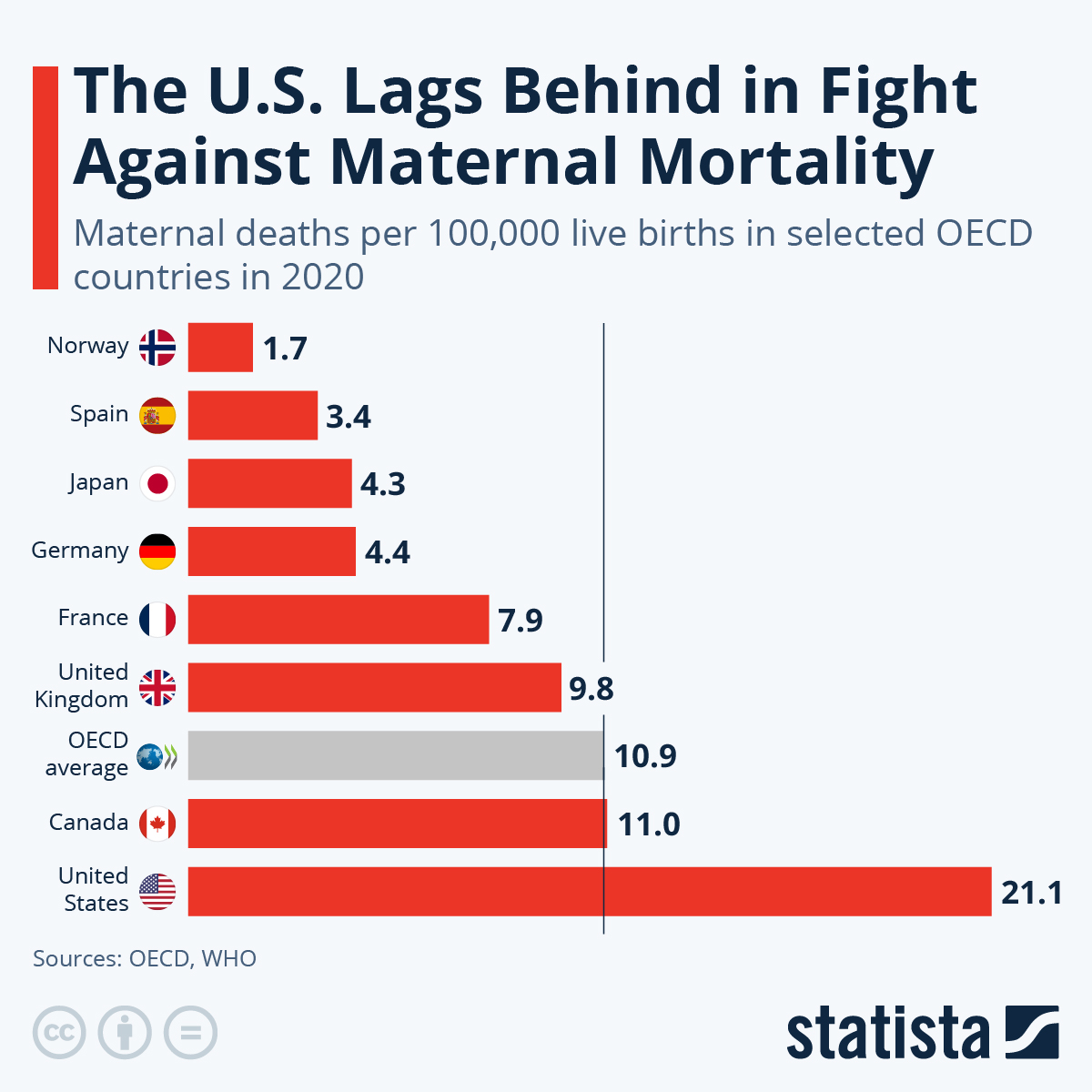
How do maternal mortality rates in the U.S. compare to those in other high-income countries?
The U.S. has the highest maternal mortality rates among high-income countries, with recent studies indicating a rise in these rates from 2018 to 2022. Many of these deaths are preventable, highlighting systemic issues within the U.S. healthcare system that differ from the more effective maternal care frameworks seen in other developed nations.
What role do postpartum care and maternal health disparities play in maternal mortality rates?
Extended postpartum care is crucial for reducing maternal mortality rates, as nearly a third of pregnancy-related deaths occur within the year following childbirth. Maternal health disparities significantly impact these outcomes, especially among racially marginalized groups, underscoring the need for policy interventions that address these inequities.
Why is cardiovascular disease a leading cause of pregnancy-related deaths in the U.S.?
Cardiovascular disease has emerged as the leading cause of pregnancy-related deaths, representing over 20% of such fatalities. This trend is linked to an increase in chronic health conditions, such as hypertension, which are being diagnosed more frequently among younger pregnant individuals, thus impacting maternal mortality rates.
How do state-level variations affect maternal mortality rates in the United States?
State-level variations in maternal mortality rates are significant, with some states exhibiting rates more than three times higher than others. This inconsistency can be attributed to differences in healthcare policies, access to care, and the quality of maternal health services, highlighting the urgent need for improved health infrastructure across states.
What is the significance of late maternal deaths in understanding maternal mortality rates?
Late maternal deaths, occurring from 42 days to one year postpartum, account for a substantial proportion of maternal fatalities. Recognizing this timeframe is essential as it indicates the need for comprehensive care strategies that extend beyond the traditional postpartum period, which is often inadequately addressed in the U.S. healthcare system.
What strategies could help reduce maternal mortality rates in the U.S.?
To effectively reduce maternal mortality rates, strategies should focus on enhancing prenatal care, improving postpartum support, and addressing systemic health inequities that contribute to maternal health disparities. Additionally, investing in public health infrastructure and promoting innovative solutions to improve care quality throughout the pregnancy continuum is crucial.
How has the COVID-19 pandemic impacted maternal mortality rates in the U.S.?
The COVID-19 pandemic is believed to have exacerbated maternal mortality rates in the U.S., with a significant rise noted in 2021. The pandemic affected healthcare access and delivery, highlighting vulnerabilities within the U.S. healthcare system that contributed to increased pregnancy-related deaths during this period.
| Key Points | Details |
|---|---|
| U.S. Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income countries, which rose from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable, yet systemic issues prevent effective healthcare delivery. |
| Disparities by Race | The mortality rate for American Indian and Alaska Native women is 106.3 deaths per 100,000 live births, much higher than white women (27.6) and non-Hispanic Black women (76.9). |
| Impact of COVID-19 | The sharpest increase in maternal mortality occurred in 2021, coinciding with the onset of the COVID-19 pandemic, though rates remain high in 2022. |
| Chronic Health Issues | There is a rising trend of chronic health issues, such as hypertension, affecting younger populations than before, contributing to mortality rates. |
| Late Maternal Deaths | Late maternal deaths (42 days to 1 year postpartum) account for nearly one-third of total maternal deaths, necessitating improved healthcare during the entire postpartum period. |
| Call for Action | Investment in public health infrastructure is needed to improve maternal health outcomes and address state-level disparities. |
Summary
Maternal mortality rates in the U.S. represent a significant public health crisis, with the country leading high-income nations in pregnancy-related deaths. Between 2018 and 2022, these rates increased alarmingly, highlighting disparities rooted in systemic inequities across various demographic groups. While many of these deaths are preventable, a lack of comprehensive care and investment in maternal health has led to dire consequences for many families. To effectively reverse this trend, it is crucial to focus on improving healthcare systems during both pregnancy and the postpartum period while addressing the racial and geographical disparities that contribute to these statistics.